Blood Cardioplegia
OBJECTIVES:To compare the cardioprotective efficacy of a solution that requires only a single infusion at the start of the ischemic duration versus a solution that requires multiple infusions. METHODS:Aortic valve replacement was performed for 150 patients, who were randomized into the del Nido (DN) cardioplegia group or the cold blood (CB) cardioplegia group. The DN cardioplegia was delivered every 90 minutes and the CB cardioplegia was delivered every 20 to 30 minutes, or whenever cardiac activity was observed. The primary endpoints were electrical cardiac activity during crossclamp, ventricular fibrillation during reperfusion, and postoperative troponin and creatine kinase (CK-MB isoenzyme) at 24 and 48 hours. RESULTS:Electrical activity during crossclamp occurred in 29 (39.7%) patients in the DN group versus 34 (45.3%) patients in the CB group (adjusted P = 1.0).
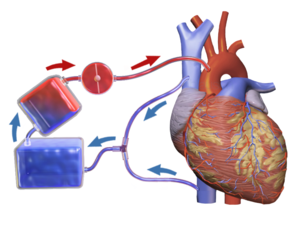
16 rows Cardioplegia plays a critical role keeping the heart protected and arrested during. The advantages of blood cardioplegia, as initially pro- mulgated, have endured and need to be only slightly modified. These were (1) rapid cardiac arrest in an oxy.
The number of procedures with ventricular fibrillation after removing the crossclamp was 41 (54.7%) in the CB group versus 17 (22.7%) in the DN group (adjusted P =.001; relative risk, 2.41). Troponin values appeared to be lower in the DN group (median, 223.10; interquartile range, 168.35-364.77 pg/mL vs 285.5; 196.20-419.45 pg/mL at 24 hours and 159.60; 125.42-217.20 pg/mL vs 201.60; 160.62-268.45 pg/mL at 48 hours) and CK-MB (median, 14.94; interquartile range, 12.16-20.39 ng/mL vs 17.43; 13.66-22.43 ng/mL at 24 hours and 6.19; 4.41-7.63 ng/mL vs 7.38; 4.74-10.20 ng/mL at 48 hours), but no significance was found. CONCLUSIONS:The del Nido cardioplegia protocol is an acceptable alternative for cold blood cardioplegia in patients undergoing aortic valve replacement.Copyright © 2019 The American Association for Thoracic Surgery. Published by Elsevier Inc. All rights reserved.
We retrospectively analyzed early results of coronary artery bypass grafting (CABG) surgery using two different types of cardioplegia for myocardial protection: antegrade intermittent warm blood or cold crystalloid cardioplegia. From January 2015 to October 2016, 330 consecutive patients underwent isolated on-pump CABG. Cardiac arrest was obtained with use of warm blood cardioplegia (WBC group, n = 297) or cold crystalloid cardioplegia (CCC group, n = 33), according to the choice of the surgeon. Euroscore II and preoperative characteristics were similar in both groups, except for the creatinine clearance, slightly lower in WBC group (77.33 ± 27.86 mL/min versus 88.77 ± 51.02 mL/min) ( P 10% was lower during each time points of evaluation, with a statistical significant difference at time 0 (4% ± 1.6% versus 5% ± 2.5%) ( P = 0.021). In presence of complete revascularization, despite the value of CK-MB/CK ratio 10% was less in the CCC group, clinical results were not affected by both types of cardioplegia adopted to myocardial protection. As compared with cold crystalloid, warm blood cardioplegia requires a shorter interval of administration to achieve better myocardial protection. Cardioplegia represents the most important strategy aimed to protect myocardial function during cardiac surgery and to facilitate surgical procedures providing a quiet and bloodless operative field.Initially, cardioplegia was introduced as an agent for hypothermic hyperkaliemic arrest.
Blood was then found to be an important vehicle for delivery of potassium cardioplegia,.Cold crystalloid cardioplegia associated with mild-to-moderate hypothermia has the advantage to decrease the oxygen consumption and offers some degree of protection during periods of low flow or low perfusion pressure. Moreover, crystalloid cardioplegia gives a better view when performing distal coronary artery anastomoses.Warm blood cardioplegia has been proposed as a safe and reliable technique for myocardial protection, based on the rationale that blood, as opposed to crystalloid solution, can potentially improve postoperative cardiac outcomes, because it more closely approximates normal physiology, i.e., carrying oxygen to the myocardium or ensuring a less hemodilution.
Nevertheless, there is still debate which is better cardioplegia for myocardial protection during cardiac surgical procedures.The aim of this study was to retrospectively evaluate whether in-hospital outcomes in patients undergoing coronary artery bypass grafting (CABG) surgery were different by using intermittent antegrade warm blood cardioplegia or intermittent antegrade cold crystalloid St. Thomas cardioplegia. From January 2015 to October 2016 at the Cardiac Surgery Unit of the Tor Vergata University Hospital of Rome, 330 consecutive patients (mean age of 67 ± 9 years) underwent isolated CABG by means of cardiopulmonary bypass. Cardiac arrest was obtained using warm blood cardioplegia (warm blood cardioplegia (WBC) group, n = 297) or cold crystalloid St. Thomas cardioplegia (crystalloid cold cardioplegia (CCC) group, n = 33) on the basis of surgeons’ choice. These two groups of patients represented the object of the present study.All patients performed preoperatively trans-thoracic echocardiography and cardiac catheterization with selective coronary angiography, and postoperatively a trans-thoracic echocardiography on the third–fourth postoperative day. Patients operated in emergency or on beating heart were excluded from the study.
The study was approved by the local Institutional Review Board, which waived the need for patient consent. This study was designed to be as retrospective one. Data collectionIn all patients were evaluated serum myocardial enzymes levels, i.e., creatine kinase (CK)-MB/CK ratio 10% and cardiac troponin I, at the end (time 0, i.e., at the admission in intensive care unit), 24 and 48 h after CABG. Perioperative myocardial infarction was defined as an increase of postoperative troponin I above10 ng/mL associated with an increase of serum CK-Muscle/Brain (MB) enzyme.10% of the total creatine-kinase enzyme, and the onset of electrocardiogram anomalies.Complete revascularization was defined when each of three major vascular territories subtended by a significant coronary artery stenosis was grafted. Postoperative low-output cardiac syndrome was defined by a cardiac index value 48 h, re-intubation, or intermittent application of non-invasive positive-pressure ventilation; permanent neurological complication due to focal or general cerebral lesion was defined as a stroke; transient ischemic attack was defined when neurological symptoms lasted.
Preoperative characteristics of the two groups are presented in Table. Both groups were similar for the preoperative characteristics, except for the clearance of creatinine, that was lower in WBC group ( P = 0.045). Intraoperative data are summarized in Table.
Aortic cross-clamp and cardiopulmonary bypass times were similar in both groups. As expected, as compared with CCC group, the mean number of cardioplegia’s doses per patient was higher in WBC group (2.0 ± 0.7 versus 2.3 ± 0.8; P = 0.045), despite the mean number of distal coronary artery anastomoses per patient was lower in WBC group (2.7 ± 0.8 versus 3.2 ± 0.9; P = 0.001).
However, complete revascularization was achieved in all patients of both groups. Operative mortality was 1.8% ( n = 6); it was 2% ( n = 6) in WBC group, and absent in CCC group ( P = not significant). Three deaths were due to cardiac causes, one death to mesenteric ischemia, two deaths to septic shock associated with multi-organ failure, respectively.Overall, serum levels of myocardial enzymes (i.e., CK-MB/CK ratio 10% and cardiac troponin I levels, at time 0, 24, and 48 h after CABG operation, respectively) were substantially similar in both groups. In particular, as compared with WBC group, CK-MB/CK ratio 10% was lower during each time points of evaluation in CCC group, with a slight statistical significant difference only at time 0 (4% ± 1.6% versus 5% ± 2.5%) ( P = 0.021) (Fig. Cardiac troponine I release was similar in all times of measurements (Fig. ). In both groups, the mean number of blood transfusion units required per patient was similar (Table ).In the same way, the incidence of perioperative myocardial infarction, low cardiac output syndrome, stroke, acute kidney injury, pulmonary complications, re-exploration for bleeding, atrio-ventricular blocks requiring need for pacemaker implantation, and the postoperative length of stay were similar in both groups ( P = not significant, for all comparisons). As compared with CCC group, the incidence of postoperative paroxysmal atrial fibrillation was higher in WBC group (33% versus 18%), although this difference did not reach a statistical significance ( P = 0.09).Postoperatively, the mean value of left ventricular ejection fraction was similar in both groups.
Protection method safety during cardiac surgery is determined by the absence of the muscular damage, i.e., impairment of ventricular contraction, and avoidance of increased myocardial enzymes, i.e., perioperative myocardial infarction. The improvement of techniques of myocardial preservation has contributed greatly to significant advances in cardiac surgery.
However, several questions remain opened regarding the use of warm versus cold cardioplegia, blood versus crystalloid cardioplegia, antegrade versus retrograde delivery, and intermittent versus continuous perfusion,.The debate over the optimal temperature of cardioplegia during cardiac surgery has been one of the most important aspects of myocardial protection. Early cardioplegic techniques used cold crystalloid solutions to initiate and maintain cardiac arrest during heart surgery, and it remained as a cornerstone of cardiac surgical practice since its introduction in the early 1950s. Although it could lower myocardial oxygen demands and consequently the risk of ischemic damage, cold cardioplegia might inhibit myocardial enzymes and it may result in the delay in metabolic and functional cardiac recovery after surgery.
In the hope of maximizing intra-operative myocardial protection, warm blood cardioplegia was first introduced in 1970s. Intermittent perfusions of warm blood cardioplegia were introduced in 1980s and proved to provide excellent myocardial protection during heart surgery,.Numerous randomized controlled trials have been conducted to compare warm cardioplegia with cold cardioplegia for myocardial protection, but the outcomes of these studies remain inconclusive.Fan et al. In a meta-analysis identifying 41 randomized controlled trials including 5897 patients, compared warm cardioplegia with cold cardioplegia for myocardial protection in patients undergoing heart surgery. The risk of in-hospital death and myocardial infarction was similar in both groups.Low-output cardiac syndrome caused by cardiac damage from inadequate myocardial preservation is a strong predictor of both perioperative and late death, and it could also prolong hospital stay and costs.
The Warm Heart Trial reported that fewer incidence of postoperative low-output syndrome occurred in the warm cardioplegia group; however, the results from previous mentioned meta-analysis did not show statistical difference between these two types of cardioplegia. Moreover, in the same way, the incidence of stroke and postoperative atrial fibrillation was similar.
The main differences of results emerging from the meta-analysis was the reduction in postoperative CK-MB and cardiac troponin concentration with the use of warm cardioplegia as compared with cold.In another meta-analysis, Guru et al. Analyzed data from 4316 patients who underwent cardiac surgery procedures using blood (cold, tepid, or warm) or cold crystalloid cardioplegia. In their analysis, blood cardioplegia provided superior myocardial protection as compared with crystalloid cardioplegia in terms of reduced incidence of low-output syndrome and reduced CK-MB release, although the incidence of death, myocardial infarction, and low cardiac output syndrome were found to be similar.In two more recently published meta-analyses performed by Abah et al. And by Zeng et al., respectively, on 5897 and 2866 patients undergoing cardiac surgery, the conclusions were different: in the first one, warm and cold cardioplegia resulted in similar short-term mortality and clinical outcomes, in the last one, cold blood cardioplegia reduced the incidence of perioperative myocardial infarction in comparison with cold crystalloid cardioplegia.
On 123 patients undergoing combined valve (aortic or mitral) and coronary artery bypass surgery found a significant reduced release in AST enzyme in favor of cold blood cardioplegia in comparison with cold crystalloid or with the use of ischemic cardiac arrest. Ascione et al. Found a significant reduced release of cardiac troponine I at 1, 24, 48 h postoperatively in favor of cold blood cardioplegia in comparison with warm blood cardioplegia.The main limitations of all the reported studies were related to the fact that the patient populations were heterogeneous, as they underwent different procedures of cardiac surgery and not isolated CABG, and that the analyzes were carried out at the same time with the use of cardioplegia warm or cold, blood, or crystalloid, administered intermittently or continuously, retrograde or antegrade,.Fiore et al. We have observed that in the presence of a complete revascularization of coronary territories, in-hospital results were not affected by the use of two different types of antegrade intermittent cardioplegia frequently used in the clinical practice to achieve the cardiac arrest during on-pump CABG.
Both strategies appear to allow an equivalent and a satisfactory method for myocardial protection during the period of cardiac arrest. As compared with cold crystalloid, warm blood cardioplegia requires a shorter interval of administration to achieve better myocardial protection. Therefore, the choice of one type of cardioplegia respect to each other remains at discretion of the surgeon. 1.Buckberg, G.
& Athanasuleas, C. Cardioplegia: solution or strategies? 50, 787–791 (2016). 2.Flack, J. Does cardioplegia type affect outcome and survival in patients with advanced left ventricular dysfunction?
Results form the CABG patch trial. Circulation 102(Suppl III), III-84–III-89 (2000). 3.Barner, H. Blood cardioplegia: a review and comparison with crystalloid cardioplegia.
52, 1354–1367 (1991). 4.Ghazy, T., Allham, O., Ouda, A., Kappert, U. & Matschke, K.
Is repeated administration of blood-cardioplegia really necessary? 8, 517–523 (2009). 5.Durandy, Y. Is there a rationale for shot cardioplegia re-dosing intervals? 7, 658–664 (2015).
6.Elvenes, O. P., Korvald, C., Myklebust, R. Warm retrograde blood cardioplegia saves more ischemic myocardium but may cause a functional impairment compared to cold crystalloid. 22, 402–409 (2002). 7.Jacquet, L.
Randomized trial of intermittent antegrade warm blood versus cold crystalloid cardioplegia. 67, 471–477 (1999). 8.Follette, D. M., Steed, D. L., Foglia, R. & Buckberg, G. Reduction on postischemic myocardial damage by maintaining arrest during initial reperfusion.
Forum 28, 281–283 (1977). 9.Rosenkranz, E. R., Buckberg, G. Warm induction of cardioplegia with glutamate-enriched blood in coronary patients with cardiogenic shock who are dependent on inotropic drugs and intra-aortic balloon support: initial experience and operative strategy. Cardiovasc Surg. 86, 507–518 (1983). 10.Ikonomidis, J.
Warm blood cardioplegia: what happens when you turn it off? Circulation 86(Suppl. 1), 103 (1992). 11.Ibrahim, M. E., Young, C.
& Chambers, D. A clinical comparative study between crystalloid and blood-based St Thomas’ hospital cardioplegic solution.
Retro city rampage apk. 15, 75–83 (1999). 12.Edelman, J. Custodiol for myocardial and preservation: a systematic review.
2, 717–728 (2013). 13.Barboza de Oliveira, M. A., Brandi, A. & dos Santos, C. Modes of induced cardiac arrest: hyperkalemia and hypocalcemia – literature review. 29, 432–436 (2014). 14.Fan, Y., Zhang, A.-M., Xiao, Y.-B., Weng, Y.-G.
Warm versus cold cardioplegia for heart surgery: a meta-analysis. 37, 912–919 (2010). 15.The Warm Heart Investigators. Randomized trial of normothermic versus hypothermic coronary artery bypass surgery. Lancet 343, 559–563 (1994). 16.Guru, V., Omura, J., Alghamdi, A. A., Weisel, R.
Is blood superior to crystalloid cardioplegia? A meta-analysis of randomized clinical trials. Circulation 114(Suppl I), I-331–I-338 (2006). 17.Abah, U., Roberts, P. G., Ishaq, M.
& De Silva, R. Is cold or warm cardioplegia superior for myocardial protection? 14, 848–855 (2012). 18.Zeng, J. Cold blood versus crystalloid cardioplegia for myocardial protection in adult cardiac surgery: a meta-analysis of randomized controlled studi.